Blood Pressure: A Comprehensive Overview
Blood pressure is a vital sign that reflects the force of blood against the walls of the arteries as the heart pumps it around the body. It is a crucial indicator of cardiovascular health, with significant implications for overall well-being. This comprehensive overview will delve into the definitions, measurements, types, causes, symptoms, diagnosis, treatment, and management of blood pressure, along with its impact on public health.
Understanding Blood Pressure
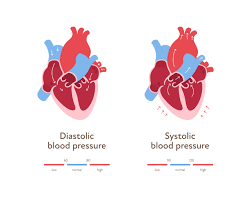
Blood pressure is expressed in millimeters of mercury (mmHg) and is recorded as two numbers:
- Systolic Pressure: The higher number, representing the pressure in the arteries when the heart beats and pumps blood.
- Diastolic Pressure: The lower number, indicating the pressure in the arteries when the heart is at rest between beats.
For example, a blood pressure reading of 120/80 mmHg means a systolic pressure of 120 mmHg and a diastolic pressure of 80 mmHg.
Normal Blood Pressure Ranges
Blood pressure categories, as defined by organizations like the American Heart Association (AHA), include:
- Normal: Systolic < 120 mmHg and Diastolic < 80 mmHg
- Elevated: Systolic 120-129 mmHg and Diastolic < 80 mmHg
- Hypertension Stage 1: Systolic 130-139 mmHg or Diastolic 80-89 mmHg
- Hypertension Stage 2: Systolic ≥ 140 mmHg or Diastolic ≥ 90 mmHg
- Hypertensive Crisis: Systolic > 180 mmHg and/or Diastolic > 120 mmHg (requires immediate medical attention)
Types of Blood Pressure
Blood pressure can be categorized based on the underlying causes and clinical presentations:
- Essential Hypertension
Also known as primary hypertension, essential hypertension accounts for about 90-95% of all cases. The exact cause is unknown, but it is believed to result from a combination of genetic, environmental, and lifestyle factors.
- Secondary Hypertension
Secondary hypertension is caused by an underlying condition, such as kidney disease, hormonal disorders, or certain medications. It accounts for about 5-10% of hypertension cases and is often more severe than essential hypertension.
- Isolated Systolic Hypertension
This condition occurs when the systolic pressure is elevated (≥ 130 mmHg) while the diastolic pressure remains normal (< 80 mmHg). It is particularly common in older adults and can be associated with an increased risk of cardiovascular events.
Causes of High Blood Pressure
The causes of hypertension can be multifactorial and may include:
Genetic Factors
A family history of hypertension increases the likelihood of developing high blood pressure, suggesting a genetic predisposition.
Lifestyle Factors
- Obesity: Excess body weight is a significant risk factor for hypertension. Fat tissue produces hormones that can elevate blood pressure.
- Physical Inactivity: Sedentary lifestyles contribute to weight gain and can lead to hypertension.
- Diet: High salt (sodium) intake, excessive alcohol consumption, and low potassium intake can increase blood pressure.
- Smoking: Tobacco use damages blood vessels and can raise blood pressure.
Medical Conditions
Certain health conditions can contribute to the development of hypertension:
- Kidney Disease: Impaired kidney function can lead to fluid retention and increased blood pressure.
- Hormonal Disorders: Conditions like hyperaldosteronism or Cushing’s syndrome can elevate blood pressure.
- Sleep Apnea: Obstructive sleep apnea is associated with higher blood pressure due to nighttime oxygen deprivation.
Symptoms of High Blood Pressure
Hypertension is often termed the “silent killer” because it usually does not present any noticeable symptoms until it reaches advanced stages. However, some individuals may experience:
- Headaches
- Dizziness
- Shortness of breath
- Nosebleeds
- Blurred vision
These symptoms may indicate severe hypertension or a hypertensive crisis, necessitating immediate medical attention.
Diagnosis of High Blood Pressure
Blood Pressure Measurement
Blood pressure is measured using a sphygmomanometer, which can be manual or automated. Accurate measurement involves:
- Proper Technique: Patients should be seated comfortably with their arm supported, and the measurement should be taken after at least five minutes of rest.
- Multiple Readings: To confirm a diagnosis of hypertension, multiple readings should be taken over several days or weeks.

Additional Tests
If secondary hypertension is suspected, healthcare providers may conduct further tests, including:
- Blood Tests: To evaluate kidney function, electrolyte levels, and hormone levels.
- Urinalysis: To check for signs of kidney disease or hormonal imbalances.
- Electrocardiogram (ECG): To assess heart health and detect any underlying cardiovascular issues.
- Echocardiogram: An ultrasound of the heart may be used to assess heart structure and function.
Treatment and Management of High Blood Pressure
Lifestyle Modifications
For many individuals with hypertension, lifestyle changes are the first line of treatment:
- Dietary Changes: Adopting a heart-healthy diet, such as the DASH (Dietary Approaches to Stop Hypertension) diet, can lower blood pressure. This diet emphasizes fruits, vegetables, whole grains, lean proteins, and low-fat dairy while reducing sodium intake.
- Regular Exercise: Engaging in moderate aerobic activity for at least 150 minutes per week can help lower blood pressure and improve heart health.
- Weight Management: Losing even a small amount of weight can significantly reduce blood pressure.
- Limiting Alcohol Intake: Reducing alcohol consumption to moderate levels can improve blood pressure control.
- Quitting Smoking: Smoking cessation is crucial for overall cardiovascular health.
Medications
When lifestyle modifications are insufficient, healthcare providers may prescribe medications to manage hypertension. Common classes of antihypertensive medications include:
- Diuretics: Help the body eliminate excess sodium and water, reducing blood volume (e.g., hydrochlorothiazide).
- ACE Inhibitors: Block the action of angiotensin-converting enzyme, leading to vasodilation and decreased blood pressure (e.g., lisinopril).
- Angiotensin II Receptor Blockers (ARBs): Similar to ACE inhibitors, these block the effects of angiotensin II (e.g., losartan).
- Calcium Channel Blockers: Relax blood vessels and decrease heart rate (e.g., amlodipine).
- Beta-Blockers: Reduce heart rate and cardiac output (e.g., metoprolol).
Monitoring and Follow-Up
Regular monitoring of blood pressure is essential for effective management. Patients are often advised to:
- Keep a Blood Pressure Log: Recording daily or weekly blood pressure readings helps track progress and identify trends.
- Regular Medical Check-Ups: Follow-up appointments with healthcare providers are vital for evaluating treatment efficacy and adjusting medications if necessary.
Complications of High Blood Pressure
Uncontrolled hypertension can lead to severe health complications, including:
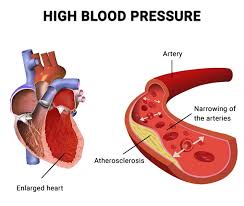
Cardiovascular Disease
Hypertension is a major risk factor for heart disease, stroke, and heart failure. High blood pressure can cause damage to the arteries, leading to atherosclerosis and increasing the risk of heart attacks.
Kidney Damage
Hypertension can impair kidney function and lead to chronic kidney disease (CKD). Over time, this can result in kidney failure, requiring dialysis or transplantation.
Vision Loss
High blood pressure can damage the blood vessels in the eyes, leading to hypertensive retinopathy and potentially resulting in vision loss.
Cognitive Decline
Hypertension is associated with an increased risk of cognitive decline and dementia, likely due to reduced blood flow to the brain.
Blood Pressure and Public Health
Hypertension is a significant public health concern globally. The World Health Organization (WHO) estimates that hypertension affects over 1.4 billion adults worldwide, with a substantial proportion being undiagnosed or untreated.
Awareness and Education
Public health initiatives focus on raising awareness about hypertension, encouraging regular blood pressure screenings, and promoting healthy lifestyle choices. Education campaigns aim to inform individuals about the risks of high blood pressure and the importance of early detection and management.
Policy Interventions
Policies aimed at reducing sodium intake in the food supply, promoting physical activity, and improving access to healthy foods can have a substantial impact on hypertension rates. Community programs that encourage healthy living and provide resources for weight management and dietary changes are vital.
Conclusion
Blood pressure is a critical measure of cardiovascular health, with significant implications for overall well-being. Understanding the complexities of hypertension—including its types, causes, symptoms, diagnosis, and management—is essential for effective prevention and treatment. With proper lifestyle modifications, regular monitoring, and appropriate medical interventions, individuals can control their blood pressure and reduce the risk of complications. Ongoing public health efforts are crucial in addressing the hypertension epidemic and promoting healthier communities.

