Cervical Cancer: A Comprehensive Overview 
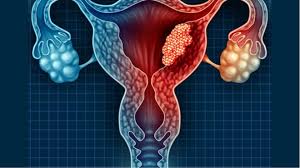
Cervical cancer is a significant public health concern and one of the most common cancers affecting women worldwide. It originates in the cervix, the lower part of the uterus that connects to the vagina. Understanding cervical cancer involves examining its causes, risk factors, symptoms, diagnosis, treatment, prevention, and its broader impact on women’s health.
Understanding Cervical Cancer
Cervical cancer occurs when the cells of the cervix undergo abnormal changes and begin to grow uncontrollably. The disease is primarily caused by persistent infection with high-risk types of human papillomavirus (HPV), a common sexually transmitted infection.
Types of Cervical Cancer
There are two main types of cervical cancer:
- Squamous Cell Carcinoma: This type accounts for about 70-90% of cervical cancer cases. It arises from the squamous cells that line the cervix.
- Adenocarcinoma: This type originates from the glandular cells of the cervix and makes up about 10-30% of cases. Its incidence has been increasing in recent years.
Stages of Cervical Cancer
Cervical cancer is staged based on how far it has spread:
- Stage 0: Carcinoma in situ, where abnormal cells are found only in the cervix.
- Stage I: Cancer has invaded the cervix but not beyond.
- Stage II: Cancer has spread to the upper two-thirds of the vagina or the surrounding tissues.
- Stage III: Cancer has spread to the lower third of the vagina, pelvic wall, or nearby lymph nodes.
- Stage IV: Cancer has spread to nearby organs (IVA) or distant organs (IVB).
Causes and Risk Factors
Human Papillomavirus (HPV)
The primary cause of cervical cancer is persistent infection with high-risk strains of HPV, particularly HPV 16 and 18. While many women are infected with HPV, the immune system typically clears the virus. However, in some cases, the virus can persist and lead to cellular changes that may develop into cancer over time.
Other Risk Factors
Several additional factors can increase the risk of developing cervical cancer:
- Age: Most cases occur in women over 30, with the highest rates in those aged 45-54.
- Smoking: Tobacco use has been linked to cervical cancer, as it can damage the DNA of cervical cells.
- Immunosuppression: Women with weakened immune systems, such as those with HIV/AIDS, are at greater risk.
- Long-term Use of Oral Contraceptives: Women who use oral contraceptives for five years or more may have an increased risk.
- Multiple Sexual Partners: Having many sexual partners increases the likelihood of HPV exposure.
- Early Sexual Activity: Engaging in sexual activity at a young age can increase the risk of HPV infection.
- History of Sexually Transmitted Infections (STIs): A history of STIs can elevate the risk of cervical cancer.
Symptoms of Cervical Cancer
In the early stages, cervical cancer may not present noticeable symptoms. As the disease progresses, women may experience:
- Abnormal Vaginal Bleeding: This can include bleeding between periods, after intercourse, or after menopause.
- Unusual Vaginal Discharge: Discharge may be watery, bloody, or have a foul odor.
- Pelvic Pain: Persistent pain in the pelvic region, especially during intercourse.
- Urinary Symptoms: Such as pain during urination or blood in the urine, if the cancer has spread.
Diagnosis of Cervical Cancer
Early detection is crucial for effective treatment and improved outcomes. The following methods are commonly used for diagnosing cervical cancer:
- Pap Smear (Pap Test)
This screening test involves collecting cells from the cervix to identify precancerous changes or cancer. The Pap test can detect abnormalities that may require further investigation.
- HPV Testing
This test checks for the presence of high-risk HPV strains. HPV testing is often done simultaneously with the Pap smear in women over 30.
- Colposcopy
If the Pap smear or HPV test results are abnormal, a colposcopy may be performed. This procedure uses a magnifying instrument to closely examine the cervix and, if necessary, take a biopsy of suspicious areas.
- Biopsy

A biopsy involves removing a small sample of cervical tissue for laboratory analysis. There are several types of biopsies, including:
- Punch Biopsy: A small section of tissue is removed using a special instrument.
- Endocervical Curettage: Cells are scraped from the inside of the cervix.
- Cone Biopsy: A larger, cone-shaped section of the cervix is removed for examination.
- Imaging Tests
If cervical cancer is diagnosed, imaging tests such as CT scans, MRIs, or PET scans may be conducted to determine the extent of the disease and whether it has spread to other parts of the body.
Treatment of Cervical Cancer
The treatment approach for cervical cancer depends on various factors, including the stage of the cancer, the patient’s overall health, and personal preferences. Common treatment options include:
- Surgery
- Conization: Removal of a cone-shaped section of the cervix, often used for early-stage cancer.
- Hysterectomy: Removal of the uterus and cervix. This may be radical (including surrounding tissues) or simple (only the uterus and cervix).
- Pelvic Exenteration: In advanced cases, removal of the uterus, cervix, and nearby organs.
- Radiation Therapy
This treatment uses high-energy rays to kill cancer cells. It can be administered externally or internally (brachytherapy). Radiation therapy may be used:
- As a primary treatment for early-stage cervical cancer.
- After surgery to eliminate remaining cancer cells.
- For advanced stages to relieve symptoms.
- Chemotherapy
Chemotherapy involves the use of drugs to kill cancer cells or stop their growth. It is often used in conjunction with radiation therapy for advanced cervical cancer or when surgery is not an option.
- Targeted Therapy and Immunotherapy
Targeted therapies focus on specific characteristics of cancer cells, while immunotherapy helps the body’s immune system fight cancer. These treatments are typically used for advanced cases and are an area of ongoing research.
Prevention of Cervical Cancer
Prevention is key in reducing the incidence of cervical cancer. Effective strategies include:
- HPV Vaccination
The HPV vaccine protects against the most common high-risk HPV types associated with cervical cancer. The vaccination is recommended for preteens (boys and girls) aged 11-12 but can be given up to age 26 or older in some cases.
- Regular Screening
Routine Pap smears and HPV testing are crucial for early detection of precancerous changes and cervical cancer. The ACOG recommends:
- Pap smear every three years for women aged 21-29.
- Pap smear and HPV testing every five years for women aged 30-65, or Pap smear alone every three years.
- Safe Sexual Practices
Practicing safe sex by using condoms and limiting the number of sexual partners can reduce the risk of HPV infection.
- Lifestyle Modifications

Maintaining a healthy lifestyle, including a balanced diet, regular exercise, and avoiding tobacco, can improve overall health and reduce cancer risk.
The Impact of Cervical Cancer on Women’s Health
Cervical cancer significantly affects women’s health globally, with disparities in incidence and mortality rates observed across different populations. The World Health Organization (WHO) estimates that in 2020, approximately 604,000 women were diagnosed with cervical cancer, and about 342,000 died from the disease.
Global Disparities
Cervical cancer is more prevalent in low- and middle-income countries, where access to screening and vaccination programs may be limited. Factors contributing to these disparities include:
- Lack of Access to Healthcare: Limited availability of screening and treatment services.
- Cultural Barriers: Stigma surrounding reproductive health and cancer may discourage women from seeking care.
- Economic Constraints: Financial barriers can prevent women from accessing preventive and treatment services.
Survivorship and Quality of Life
Survivors of cervical cancer may face long-term physical and emotional challenges, including:
- Physical Effects: Changes in sexual function, bowel and urinary problems, and menopause symptoms may occur after treatment.
- Emotional Impact: Anxiety, depression, and concerns about body image and fertility are common among survivors.
Support services, counseling, and survivorship programs can help address these challenges and improve quality of life for survivors.
Conclusion
Cervical cancer remains a significant global health issue, but it is largely preventable through vaccination, regular screening, and healthy lifestyle choices. Understanding the causes, symptoms, diagnosis, and treatment options is crucial for early detection and effective management. Ongoing public health efforts are essential to improve access to prevention and treatment, particularly in underserved populations. With continued awareness and education, cervical cancer can be significantly reduced, leading to healthier outcomes for women worldwide.